HEAD & NECK RECONSTRUCTION
ABOUT
Head & Neck Reconstruction
Head & Neck Reconstruction is restoring essential functions and form after cancer resection.
Head and neck cancers can leave significant defects after surgical removal, affecting vital functions such as speech, breathing, and feeding. The anatomy of this region is complex, and reconstruction aims to restore both function and form while minimising additional surgical impact.
PROCEDURES
What Can Be Reconstructed
Scalp & Cranial Defects
Small to moderate defects may be reconstructed using local flaps from the scalp. Larger defects may require free tissue transfer from the thigh or back.
Cranial defects may be reconstructed using bone grafts or patient-specific 3D-printed implants.
Nasal Defects
Most nasal defects from skin cancers are reconstructed with local facial flaps to minimise scarring and preserve nasal function. Larger defects may require a paramedian forehead flap or free-tissue transfer.
Orbit & Cheek Defects
Resection of tumours around the eye or maxillary area may require complex reconstruction to restore cheek projection, eye support, and feeding function. Tissue flaps from the thigh or fibula may be used depending on the defect.
Oral Defects – Tongue & Jaw
Tongue cancers affect swallowing, speech, and breathing. Reconstruction may involve reshaping forearm or thigh tissue into a neo-tongue. Jaw reconstruction may use a fibula flap shaped into a neo-mandible using 3D planning technology.
How Reconstruction Is Planned & Performed
What Are Flaps?
Flaps are units of tissue – skin, fat, bone, and sometimes nerves with their own blood supply. Smaller defects may be reconstructed with local flaps, while larger ones may require free tissue transfer from donor sites such as the forearm, groin, thigh, leg, or intestine.
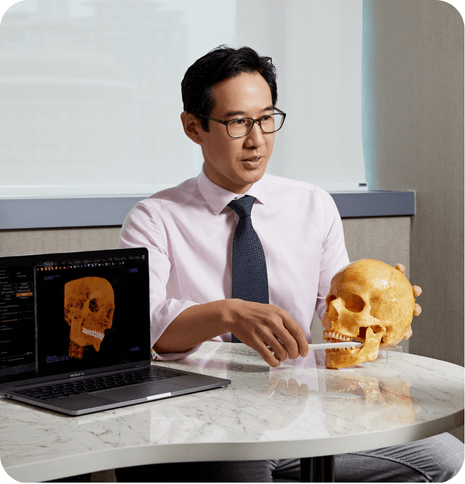
Pre-Surgery Planning
Reconstruction is planned closely with the head and neck cancer resection team. CT scans and computer‑assisted planning help identify missing tissue components and design precise reconstruction. Blood tests and anaesthetist reviews are also part of preparation.
INDICATIONS
Who May Need Reconstruction?
Patients undergoing surgical removal of head and neck cancers that result in functional or structural defects.
SAFETY
Risks & Considerations
- Bleeding requiring transfusion
- Infections
- Flap complications or flap failure
- Need for secondary flap reconstruction
- Revision procedures
- Scars at donor and recipient sites
- Facial asymmetry
- Loss of critical functions (speech, swallowing, or breathing)
- Complications from prolonged bed rest
- Complications related to anaesthesia
AFTERCARE
Downtime & Recovery

- Hospitalisation typically lasts 1–2 weeks.
- Initial monitoring may occur in the intensive care unit or high-dependency ward.
- There may be drains at the donor and recipient sites, as well as tubes to support breathing and feeding. These are removed as recovery progresses.
- Physiotherapists will assist with rehabilitation, including speech and swallowing therapy for tongue reconstruction and mobility training for donor site recovery.
HOW TO START
Arrange a Consultation
If you are considering the treatment with our experienced surgeons, you may book a consultation to discuss suitability, options, and the treatment process based on your medical history and goals.
FAQ
Frequently Asked Questions
How long will I be in hospital?
Most patients stay 1–2 weeks depending on the extent of surgery and complexity of reconstruction.
What support will I receive during recovery?
Physiotherapists will assist with rehabilitation, including speech and swallowing therapy for tongue reconstruction and mobility training for donor site recovery.
🩺 A full evaluation with an MOH-accredited doctor is required to determine suitability for the procedure.
*Disclaimer: Results vary according to individual.
GET IN TOUCH
Book Your Consultation